Stratified squamous epithelium is one of those structures in biology that, well, gets overlooked in favor of cooler-sounding tissues—but it’s actually pretty essential. We sense textures, shield ourselves from rugged environments, and maintain moisture all thanks to this multi-layered cell carpet. It’s not flashy, but it’s reliable—a bit like that dependable friend who has your back when things get messy. This piece dives into what it is, where it is, why it matters, and how researchers and clinicians pay attention to its quirks in real-world scenarios.
What Is Stratified Squamous Epithelium?
Stratified squamous epithelium consists of several layers of flattened cells, making it robust against mechanical stress and dehydration. In plain terms, imagine stacking sheets of paper—each sheet represents a cell layer, together forming a sturdy barrier. This layered arrangement helps tissues resist abrasion and maintain integrity, especially where there’s friction or potential exposure. The topmost cells may be keratinized (as in skin) for extra protection or non-keratinized (as in mouth lining) to retain moisture.
Structural Highlights
- Multiple cell layers provide physical durability.
- Keratinization adds a toughened, water-resistant surface—skin, for example, shows this trait.
- Non-keratinized regions stay moist and flexible, as seen in oral mucosa or esophagus.
Where It’s Found in the Body and Why Location Matters
Keratinized Regions: The Skin’s Armor
In areas exposed to the environment—think palms, soles, or scalp—the stratified squamous epithelium becomes keratin-rich. This keratin layer shields against physical trauma, pathogens, and water loss. It’s like wearing reinforced armor that still lets you move freely. You don’t realize it’s working until you scrape your knee, then suddenly, that barrier feels pretty darn important.
Non-Keratinized Regions: Internal Moisture-Retaining Lining
Continuing inward, certain surfaces call for a softer touch. The mouth, throat, esophagus, and vaginal lining rely on non-keratinized stratified squamous epithelium. It’s protective, yet flexible and keeps tissues from drying out. It’s sort of like the difference between the back of a velvet glove and the grit of a sandpaper palm.
Roles & Real-World Significance
Protection and Resilience
These tissues act as frontline defenders. Consider, say, a dentist probing teeth or someone gulping a sandwich—that movement and contact could damage a simpler, single-layer epithelium. Instead, the stratified variety absorbs and dissipates pressure. Over time, it adapts through natural keratin accumulation or cellular turnover, reinforcing areas that undergo repetitive stress.
Moisture Regulation and Self-Repair
In non-keratinized zones, this epithelium cleverly balances moisture and durability. The cells glom together tightly, preventing drying but allowing enough flexibility for speech, swallowing, and other motions. When injury strikes—like a canker sore—cell renewal kicks in fast. The layered setup lets the deeper, healthier cells push upward and fill in the gap smoothly.
Clinical and Research Contexts
Clinicians frequently assess stratified squamous epithelium in diagnostic contexts. For example, pathologists examine samples from the cervix for dysplasia—precancerous changes—in non-keratinized areas. In skin research, investigations into barrier repair, eczema, or psoriasis often focus on keratinized stratified squamous layers. It’s a significant model system for understanding not only mechanical resilience but scales of inflammation and healing dynamics.
“Understanding how stratified squamous epithelium behaves under stress isn’t just academic—it’s foundational for treating wounds, managing skin diseases, and anticipating changes in mucosal health.”
Layers and Cellular Dynamics
The Layer Breakdown
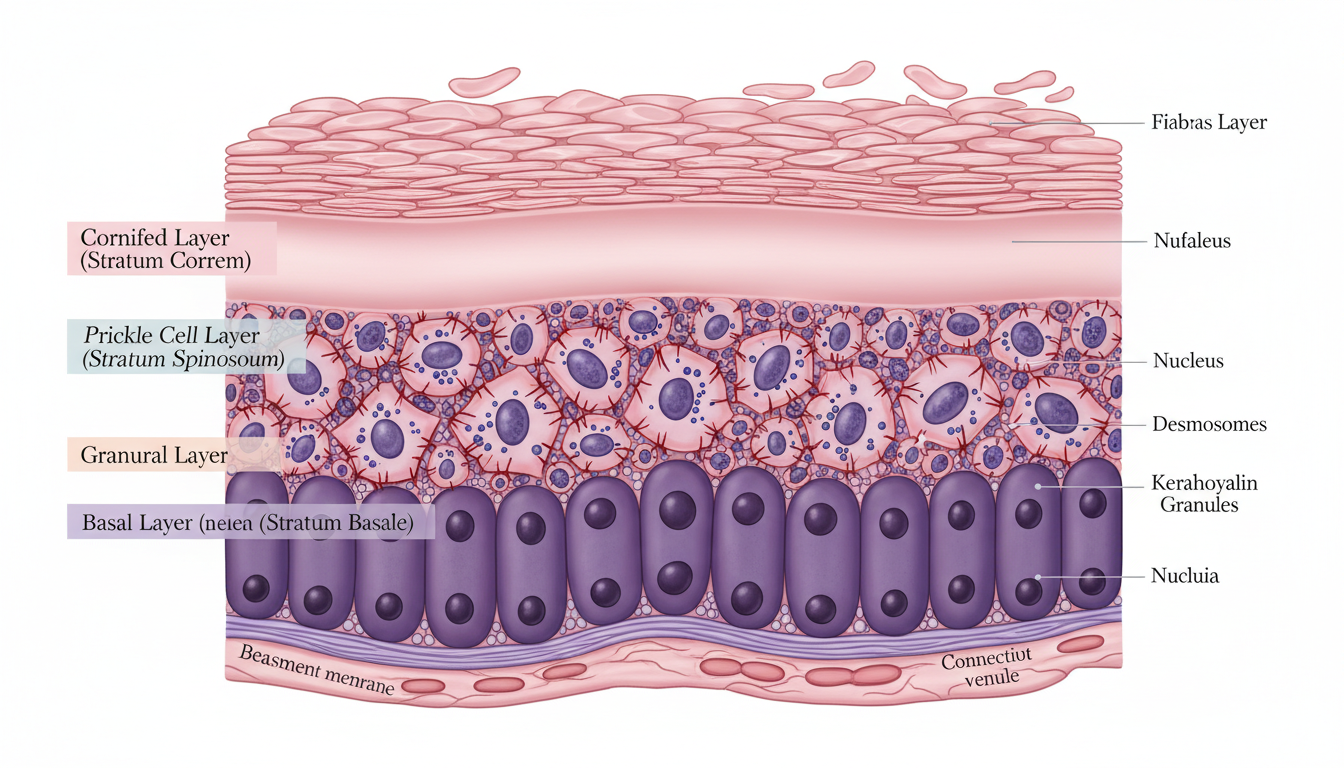
Although simplified, here’s a quick breakdown of the cellular stack:
- Basal layer: Home to stem-like cells that divide and give rise to new layers.
- Intermediate layers: Cells enlarge and flatten, migrating upward, slowly giving up their vitality.
- Superficial layer: Either dead, keratin-packed slabs (in skin) or living flattened cells (in mucosa).
This structure isn’t static—it’s alive, dynamic, constantly regenerating. The turnover rate varies by site; the skin might take a few weeks, while the mouth lining renews much faster, given its exposure to chewing, talking, and microbial traffic.
Why It Matters Technically
In research, stratified squamous epithelium offers a window into differentiation and cell death processes. How do basal cells know when to divide? Why do some cells keratinize fully and others don’t? Insights here inform therapies for conditions from ulcers to chronic dermatitis. Moreover, tissue engineers are trying to recreate these layered patterns for grafts or lab-grown skin—operationally complex, but promising for burn victims or surgical reconstruction.
Comparative View: Stratified vs. Simple and Cuboidal Epithelia
In contrast to stratified types, simple epithelia—like that lining the small intestine—are one-cell thick, allowing rapid nutrient absorption or gas exchange. Cuboidal epithelia resemble cubes and exist in glands or ducts where secretion or filtration is key. Stratified squamous epithelium trades permeability for robustness—so it’s thicker, tougher, but less suited for tasks like absorption. Your stomach lining, for example, isn’t built for abrasion in the same way your tongue or skin is.
A Closer Look: Keratinized vs. Non-Keratinized Features
Keratinized Epithelium Details
- Rich in keratin, non-living outer layer—highly protective.
- Ideal for dry, abrasive environments.
- Slow, steady regeneration—skin can feel rough when turnover slows, as in aging.
Non-Keratinized Epithelium Insights
- Retains living superficial cells—maintains moisture.
- Excellent for internal passageways or areas needing flexibility.
- Quickly adaptable; heals more rapidly after injury, provided moisture and blood supply are adequate.
Practical Applications and Study Cases
Wound Healing Scenario
Imagine a minor scrape on your arm—keratinized epithelium gets breached, but underlying basal cells begin replicating; eventually they migrate, re-keratinize the surface, and restore the barrier. It’s not instant, but the layered design makes this possible, whereas a simpler tissue would struggle or scar more unpredictably.
Oral Health Case
Think about biting your inner cheek—OUCH! The non-keratinized lining handles abrasion daily, yet when injured by teeth, it regenerates rather quickly. Dentists rely on this repair tendency, knowing that light trauma heals swiftly unless the area remains irritated.
Tissue Engineering Example
Researchers have successfully grown stratified squamous epithelium in vitro for graft applications. They seed basal cells on scaffolds, coax them to differentiate, and train them under air–liquid conditions to mimic keratinization. Real-world trials, especially for burn treatment, show promise—though scaling, vascularization, and immune matching remain hurdles.
Why People Should Care
Beyond biology classes, stratified squamous epithelium matters to dermatologists, dentists, surgeons, pharmacologists, and anyone who’s ever chased wound healing or mucosal health. Understanding how this tissue works helps in:
- Designing better topical therapies
- Predicting how injuries heal
- Developing artificial skin or mucosa
- Managing conditions like leukoplakia, oral ulcers, or psoriasis
It’s quiet workhorse tissue—it doesn’t make headlines, but it keeps you intact daily.
Conclusion
In short, stratified squamous epithelium is a layered tissue marvel—built for protection, flexibility, and resilience whether it’s hardened skin or delicate oral lining. Its layered structure means it withstands stress, repairs itself, and continues doing its quiet, essential job. Researchers, clinicians, and engineers keep probing its behavior to improve treatments, mimic its dynamics, or support healing. Always available, always adaptive—this is the tissue you rely on when friction, abrasion, or dryness would otherwise do you in.
FAQs
-
What’s the difference between keratinized and non-keratinized stratified squamous epithelium?
Keratinized epithelium has a tough, protein-rich outer layer ideal for dry, abrasive areas like skin. Non-keratinized remains flexible and moist, suited for regions like the mouth or esophagus. -
How does stratified squamous epithelium regenerate?
Basal cells divide and push upward, gradually flattening and, in some cases, keratinizing. This layered renewal helps repair injuries and maintain barrier function. -
Why is this tissue important in diagnostics?
It’s commonly examined in biopsies—for example, cervical screening or assessing oral lesions—because changes in its cellular layers can signal disease progression or cancer risk. -
Can we grow stratified squamous epithelium in the lab?
Yes. Scientists culture basal cells on scaffolds and induce layering and keratinization under lab conditions. These models are useful for grafting and studying skin disorders. -
What kind of damage can it withstand?
It’s resistant to friction, pressure, and dehydration—keratinized forms especially so. Non-keratinized forms endure moisture-rich movement and repair quickly after minor trauma. -
How does this tissue differ from simple epithelial types?
Unlike single-cell-thick simple epithelium that absorbs or filters quickly, stratified squamous epithelium is thick, durable, and protective—but slower in exchange or absorption roles.


 February 7, 2026
February 7, 2026  7 Min
7 Min  No Comment
No Comment